The journey to parenthood is often portrayed as straightforward. However, for millions of couples worldwide, it is filled with unexpected challenges and emotional complexities. If you have been trying to conceive for a year or more without success (or six months if you are over 35), you may be experiencing subfertility. Understanding the causes of subfertility is the crucial first step toward finding effective solutions and reclaiming control over your reproductive health. This comprehensive guide will explore the ten most common causes of subfertility, detailing each one, discussing potential treatment options, and empowering you with the knowledge needed for an informed conversation with a fertility specialist.
What is Subfertility? Definition
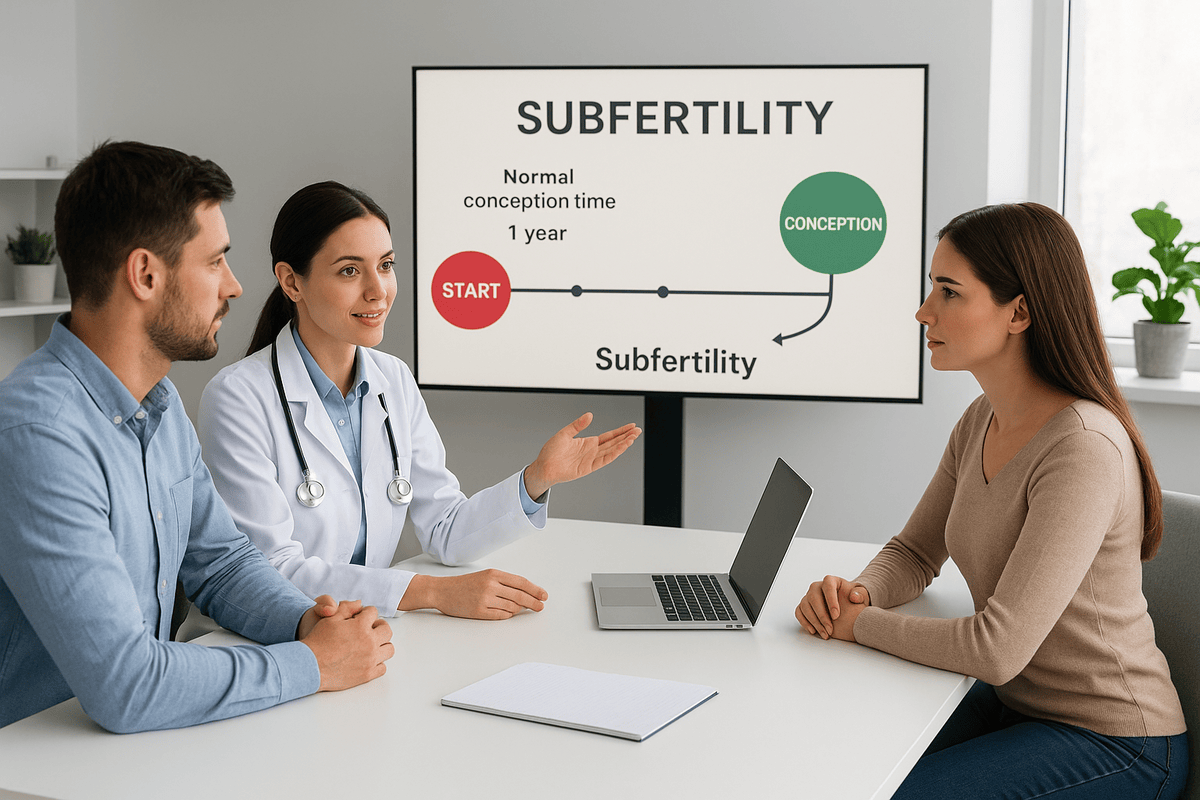
Before we delve into specific causes, it is essential to clarify the definition of subfertility. Often used interchangeably with infertility, there is a subtle but important distinction. Infertility typically refers to a complete inability to conceive, while subfertility indicates a reduced or delayed ability to conceive. In other words, a subfertile couple may still conceive naturally, but it may take longer than average. This term acknowledges that fertility exists on a spectrum and frames the situation as a medical condition with identifiable and often treatable causes. Recognizing this empowers individuals and couples to seek help proactively rather than feeling hopeless.
The Top 10 Causes of Subfertility
Identifying the root cause of subfertility is vital for effective intervention. Often, subfertility results from a combination of factors affecting both partners. Here are the ten common causes you should be aware of:
1. Ovulatory Disorders: The Foundation of Female Fertility
Ovulation, the release of a mature egg from the ovary, is central to female fertility. Any disruption in this hormonal process can lead to subfertility in women, accounting for approximately 25% of cases. Conditions like Polycystic Ovary Syndrome (PCOS) disrupt hormone balance, leading to irregular or absent periods. Other disorders such as hypothalamic dysfunction, premature ovarian insufficiency (POI), extreme stress, excessive exercise, or significant weight changes can also affect ovulation. Fortunately, many ovulatory disorders respond well to lifestyle changes and medication, making them highly treatable.
2. Male Factor Infertility: Sperm Health, Count, and Motility
It is a common misconception that fertility issues lie mainly with the female partner. In reality, male factor issues contribute to about 30-40% of subfertility cases. These include low sperm count (oligospermia), poor sperm motility (asthenospermia), abnormal sperm shape (teratospermia), or no sperm in the ejaculate (azoospermia). Factors such as genetic conditions, hormonal imbalances, past infections like mumps, varicoceles (enlarged veins in the scrotum), environmental toxins, smoking, and excessive alcohol use can all play a role. A semen analysis is a vital first step in any subfertility evaluation.
3. Tubal Factor Infertility: The Blocked Pathway
The fallopian tubes are essential for conception, as they are where sperm meets the egg. Blocked or damaged tubes lead to tubal factor infertility, a significant cause of subfertility. Pelvic Inflammatory Disease (PID), often due to untreated sexually transmitted infections like chlamydia or gonorrhea, is a primary cause of blocked tubes. Other causes include previous pelvic surgery, endometriosis, or ectopic pregnancies that damage the tubes. Diagnosing tubal blockages often requires an X-ray called a hysterosalpingogram (HSG).
4. Endometriosis: The Unwelcome Guest
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often affecting the ovaries and fallopian tubes. This tissue thickens and bleeds during the menstrual cycle but cannot exit the body, leading to inflammation and painful scar tissue (adhesions). This condition can distort pelvic anatomy, block tubes, hinder implantation, and affect egg quality. Interestingly, the severity of pain does not always correlate with the extent of the disease; even mild endometriosis can be a hidden cause of subfertility.
5. Uterine or Cervical Abnormalities: Structural Hurdles
The uterus nurtures the developing embryo, while the cervix allows sperm to pass through. Structural abnormalities in these areas can create significant challenges. Uterine issues may include congenital conditions like a septate uterus, fibroids (non-cancerous tumors that distort uterine shape), polyps, or scarring from previous procedures (Asherman’s syndrome). Cervical factors may involve surgical alterations to the cervix or an inability to produce suitable mucus for sperm transport.
6. Unexplained Subfertility: The Frustrating Diagnosis
One of the most perplexing diagnoses for couples is unexplained subfertility. This term applies when a thorough fertility evaluation, including ovulation confirmation, semen analysis, HSG, and possibly laparoscopic evaluation, fails to identify a clear cause. Unexplained subfertility accounts for about 15-30% of cases. It does not imply that there is no cause; rather, it indicates that the cause may be too subtle for current diagnostic tests to detect. This can involve issues with egg quality, sperm function, or the intricate processes of fertilization and implantation. While this diagnosis can be frustrating, it opens the door to effective treatments for subfertility. Many couples begin with less invasive options like ovulation induction combined with intrauterine insemination (IUI) before considering IVF.
7. Age-Related Fertility Decline: The Biological Clock
Female age is one of the most significant factors influencing fertility. Women are born with a finite supply of eggs, and both the quantity and quality of these eggs decline progressively with age. This decline becomes more pronounced after age 35. As women age, their eggs are more likely to have chromosomal abnormalities, which can lead to difficulties in conception, a higher risk of miscarriage, and an increased chance of genetic disorders. While male fertility also declines with age, affecting sperm quality and genetic integrity, this process is generally more gradual than in women. Understanding this biological factor is crucial for family planning and seeking timely help from a fertility specialist.
8. Lifestyle and Environmental Factors: The Controllable Variables
Your daily habits and environment significantly affect fertility. These modifiable factors are critical areas where individuals can take immediate action to improve their chances of conception. Smoking is harmful to both female and male fertility, accelerating egg depletion and damaging sperm DNA. Excessive alcohol consumption, recreational drug use, and being significantly overweight or underweight can disrupt hormonal balance. Exposure to environmental toxins, pesticides, industrial chemicals, and excessive heat (for men) can negatively impact reproductive function. Addressing these causes of subfertility through positive lifestyle changes is a powerful first step in treatment.
9. Thyroid and Other Medical Conditions: The Systemic Link
The endocrine system is a complex network of glands, and dysfunction in one area can affect others, including the reproductive system. Thyroid disorders, whether hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid), can disrupt the menstrual cycle and inhibit ovulation. Similarly, uncontrolled diabetes can impact fertility in both men and women. Other medical conditions like Cushing’s disease, sickle cell disease, and kidney disease can also contribute to subfertility. Furthermore, treatments for other illnesses, particularly certain chemotherapy and radiation therapies for cancer, can severely affect fertility. Pre-treatment consultations on fertility preservation are essential.
10. Immunological Factors: When the Body Attacks Itself
Though less common, immunological factors can also cause subfertility. This occurs when the body’s immune system mistakenly identifies sperm or the embryo as foreign invaders and attacks them. In men, an immune response can produce anti-sperm antibodies that immobilize or clump sperm together. In women, certain immune system issues may prevent the embryo from successfully implanting in the uterine lining or lead to recurrent miscarriages. This specialized area of reproductive immunology is typically investigated after ruling out more common causes of subfertility.
Diagnosis and Treatment for Subfertility: Your Path Forward
Recognizing these common causes of subfertility is the first step; the next is obtaining a formal diagnosis. A fertility specialist will conduct a systematic evaluation involving a detailed medical history, blood tests to check hormone levels, a semen analysis, an HSG to examine the tubes, and an ultrasound to assess the ovaries and uterus. The specific treatment for subfertility depends entirely on the underlying cause. Options range from simple lifestyle changes and oral ovulation-inducing drugs like Clomid to more advanced procedures. Assisted Reproductive Technology (ART) encompasses all fertility treatments that handle eggs and embryos, including:
- Intrauterine Insemination (IUI): Washed and concentrated sperm are placed directly into the uterus around ovulation.
- In Vitro Fertilization (IVF): Eggs are retrieved from the ovaries and fertilized with sperm in a lab. The resulting embryos are then transferred into the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected directly into an egg to facilitate fertilization, often used for severe male factor infertility.
When to See a Fertility Specialist: Don’t Wait to Seek Help
Time plays a crucial role in fertility. If you are under 35 and have not conceived after one year of regular, unprotected intercourse, it is time to seek help. For those 35 or older, you should consult a specialist after six months. However, do not wait if you have known issues such as irregular periods, a history of pelvic disease, painful periods, previous miscarriages, or if your partner has a known sperm issue. A fertility specialist is not only for those needing IVF; they are diagnostic experts who can guide you through the entire process, from basic testing to the most suitable treatment for your unique situation.
Learn About Sexual Narcissism
Conclusion: Empowerment Through Knowledge
The journey through subfertility can feel isolating and overwhelming, but you are not alone. Understanding the common causes of subfertility empowers you to ask the right questions, advocate for your health, and make informed decisions. Remember, subfertility is a medical condition, not a personal failure. Many couples have successfully overcome these challenges thanks to advancements in modern medicine, particularly in Assisted Reproductive Technology. By recognizing the signs, seeking timely help from a qualified fertility specialist, and exploring various treatment options, you can move forward with hope and confidence on your journey to build the family you desire.