Imagine fragile passages that were meant to carry life, now suddenly blocking and filling with fluid. This is the scary truth about hydrosalpinx, a disorder affecting the fallopian tubes. It seriously impacts a woman’s ability to have children. Hydrosalpinx is not a small problem; it is a serious diagnosis that doctors must understand and address immediately. If you don’t pay attention to it, it could ruin your chances of getting pregnant and cause major problems.
This guide explains hydrosalpinx, what it is, its causes, and key risks (especially bilateral hydrosalpinx). It also covers the essential steps for effective treatment. For you to take charge of your gynecological health, it’s important to know the answers to questions like “How serious is hydrosalpinx?” and “Is it necessary to remove hydrosalpinx?”
Understanding Hydrosalpinx: A Blockage with Consequences
Hydrosalpinx (pronounced hi-dro-SAL-pinks) is a term that refers to a specific issue in a fallopian tube. The word combines ‘hydro,’ meaning water, and ‘salpinx,’ meaning tube.” In short, fluid blocks one or both fallopian tubes. These tubes are not only passive channels; they are quite important for reproduction. The fallopian tubes catch the egg released from the ovary and create the ideal environment for fertilization. Once an embryo forms, they transport it to the uterus for implantation.
When a hydrosalpinx forms, this complicated process is significantly messed up. The tube gets bigger and fuller with a watery fluid that is usually sterile. This blockage prevents the egg and sperm from meeting. It’s a major obstacle to pregnancy. The trapped fluid isn’t just harmless; research shows it can create a toxic environment for embryos. It may also disrupt implantation, drastically reducing pregnancy success, even with IVF.
What Causes Hydrosalpinx? Tracing the Source of the Blockage
Most of the time, hydrosalpinx happens because of damage or infection that happened in the past in the pelvis. These scars and blocks the delicate ends of the fallopian tube, called the fimbriae. Finding the root cause helps us understand the disease and possible ways to address it:
- Pelvic Inflammatory Disease (PID): Pelvic Inflammatory Disease (PID) is the clear number one cause. PID, often caused by STIs like chlamydia or gonorrhea, triggers inflammation and infection in the upper reproductive tract. This can lead to scarring that blocks the tubes, trapping fluid produced by their lining. Practice safe sex and treat infections early to avoid PID.
- Endometriosis: Endometriosis is a disorder in which tissue that is comparable to the lining of the uterus grows outside the uterus. This can lead to a lot of inflammation and adhesions (scar tissue bands) in the pelvic. These adhesions can change the shape of the tubes or obstruct them, which can lead to the creation of hydrosalpinx.
- Previous Pelvic or Abdominal Surgery: Surgeries like appendectomies, ovarian cyst removals, or even tubal procedures can cause adhesions. These scar tissues may block the fallopian tubes. Surgeons take every precaution to prevent complications, but scar tissue naturally forms during healing, sometimes causing problems.
- Previous Ectopic Pregnancy: An ectopic pregnancy that happens in a fallopian tube might hurt the tube’s structure, leave scars, and obstruct it, which could lead to hydrosalpinx.
- Tuberculosis (TB): In areas where genital tuberculosis is common, it can be a major cause of tubal damage and hydrosalpinx. TB creates a certain kind of damage that causes inflammation.
- Other Infections: Sometimes, severe infections that happen after giving birth (puerperal infection) or having a miscarriage might spread and harm the tubes.
Recognizing Hydrosalpinx: Symptoms and Silent Presence
One of the hardest things about hydrosalpinx is that it can be entirely quiet. Many women remain unaware of this condition. They often only learn about it during fertility exams. When symptoms occur, they’re typically linked to the underlying cause. Alternatively, they may result from the physical pressure of the fluid-filled tube itself.
- Chronic Pelvic Pain: People often complain of dull discomfort or pressure in the lower abdomen or pelvis that doesn’t go away. This ache could be present all the time or only occasionally.
- Pain During Intercourse (Dyspareunia): You may feel deep pelvic pain during or after intercourse. The enlarged tubes or adhesions in this location typically cause discomfort.
- Watery Vaginal Discharge: Some women may have watery vaginal discharge, especially if the hydrosalpinx empties into the uterus from time to time.
- Pelvic Pain During Menstruation: Pain may get worse right before or during your period.
- Infertility: This is often the main and most serious sign that leads to a diagnosis. If you’ve been trying to get pregnant for a year (or six months if you’re over 35) and haven’t been able to, you should see a doctor. Tubal factors like hydrosalpinx are a big reason why.
Also this: Pelvic Inflammatory Disease & Fertility: Protecting Your Path to Parenthood
Why Diagnosis Matters: Detecting Hydrosalpinx
Hydrosalpinx often has no symptoms, so doctors typically diagnose it during fertility testing or pelvic pain evaluations. They use specialized imaging tests to confirm the condition.
- Hysterosalpingogram (HSG): This is usually the first test that doctors use to find out what’s wrong. The procedure involves injecting a special dye through the cervix into the uterus and fallopian tubes. As the dye pours, X-ray pictures are taken. With hydrosalpinx, the dye fills the blocked tube, revealing a swollen, sausage-like shape. Unlike healthy tubes, the dye won’t spill into the abdominal cavity. An HSG clearly shows whether one or both tubes are damaged (bilateral hydrosalpinx).
- Transvaginal Ultrasound: A trained sonographer can sometimes see fluid-filled, dilated tubes near to the ovaries, although this isn’t as clear-cut as HSG for checking if the tubes are open. If the hydrosalpinx is big, this is more likely to happen. Ultrasound is a great way to check out the pelvis for the first time.
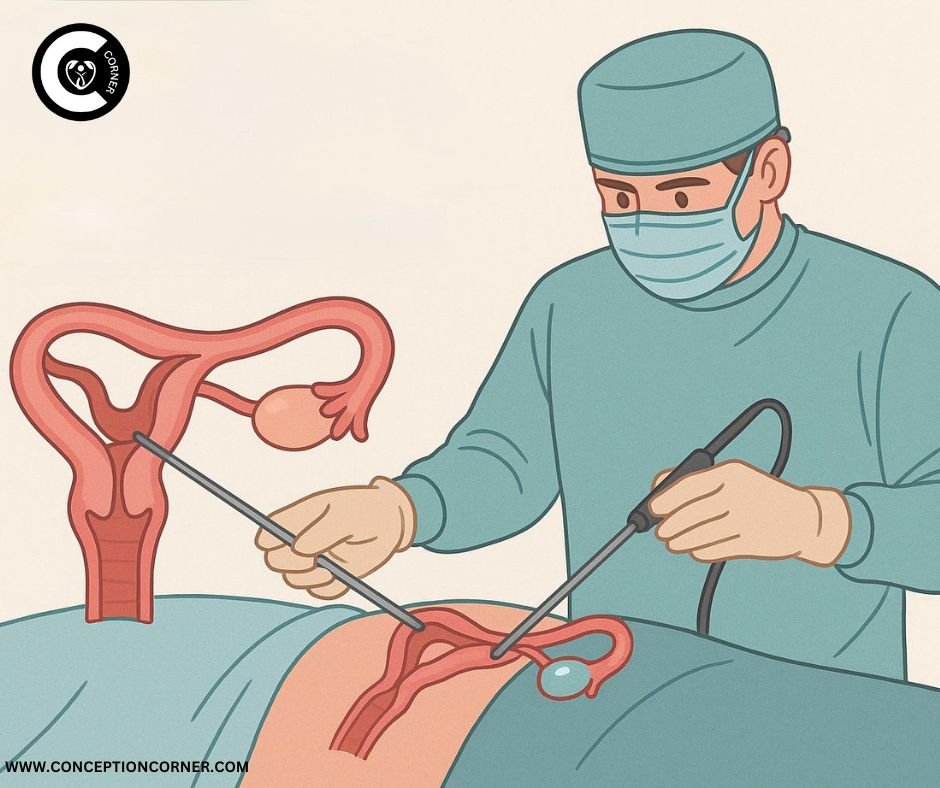
- Laparoscopy: Laparoscopy is a minimally invasive surgery that is the best way to find out if you have tubal illness or pelvic pathology like hydrosalpinx. Using a laparoscope a thin, lighted telescope, the surgeon views the reproductive organs through a small belly button incision. This allows direct examination of the tubes, ovaries, uterus, and pelvic cavity. This gives the best picture of how bad the tube is, how much damage it has, and whether there are adhesions or endometriosis. During laparoscopy, diagnosis and possible treatment (such as removal) can often happen at the same time.
- Saline Infusion Sonography (SIS or SHG): During this procedure, doctors inject sterile saline into the uterus while performing a transvaginal ultrasound. While primarily examining the uterine cavity, it can also detect blocked tubes. The test reveals whether fluid flows properly or if the tubes appear abnormally dilated.
How Serious is Hydrosalpinx? Understanding the Significant Risks
So, how bad is hydrosalpinx? The answer is clear: it is a dangerous disorder that has a big effect on fertility and general health. You can’t just ignore it. This is why:
- Profound Impact on Fertility: It has a profound effect on fertility
- Natural Conception: Hydrosalpinx physically stops the egg and sperm from meeting, making natural conception very unlikely or even impossible. Bilateral hydrosalpinx, which affects both tubes, makes it almost impossible to get pregnant naturally.
- IVF Success Rates: A hydrosalpinx harms IVF success even when the tubes aren’t involved. The fluid that is harmful inside the tube might leak back into the uterus. This is called “hydrosalpinx reflux.” This liquid can flush embryos out of the uterus. It contains germs and inflammatory compounds that are bad for embryos and lower the chances of implantation, even if the person is not actively ill. Makes the uterine lining (endometrium) less susceptible to implantation by creating an environment that is not good for it.
Studies consistently reveal that women with untreated hydrosalpinx have far lower rates of pregnancy and live birth after IVF than women who don’t have it or who have had the afflicted tube(s) removed before IVF.
- Risk of Infection and Abscess Formation: The fluid in a chronic hydrosalpinx is usually sterile, but the stagnant environment can sometimes become infected (pyosalpinx). This could cause a serious pelvic infection that needs antibiotics right away and maybe even surgery. If the infection becomes worse, it can turn into a tubo-ovarian abscess (TOA), which is a painful and hazardous buildup of pus in the tube and ovary. People with TOAs often need to stay in the hospital, get IV antibiotics, and have their abscess drained or surgically removed.
- Ectopic Pregnancy Risk: Even if an egg fertilizes despite a partial blockage near a hydrosalpinx, the damaged tube often fails to transport the embryo properly. This makes it much more likely that the embryo will implant in the tube itself, which would lead to an ectopic pregnancy. Ectopic pregnancies are medical emergencies that can break open and cause life-threatening internal bleeding. A history of hydrosalpinx or injury to the tubes is a big risk factor.
Hydrosalpinx Rupture Symptoms: Recognizing a Rare but Critical Emergency
A large hydrosalpinx can break, but this is rare, just like an ovarian cyst might break. This is a critical acute occurrence that needs medical intervention right away. It’s important to know the signs of a hydrosalpinx rupture:
- Severe, sudden pelvic or abdominal pain: This pain is usually quite strong and severe, and people often say it feels like “stabbing” or “tearing.” The pain could start on one side, but it might spread to the whole body.
- Significant Worsening of Chronic Pain: A sudden, big rise in baseline pelvic discomfort that makes chronic pain much worse.
- Nausea and Vomiting: Nausea and vomiting are common reactions to acute pain and discomfort inside the body.
- Fever and chills: These could be signs of an infection or inflammation caused by the spilled fluid.
- Lightheadedness, Dizziness, or Fainting: These could be indicators of internal bleeding or a systemic inflammatory response, like early sepsis.
- Pain in the shoulder tip: If fluid or blood leaks out and irritates the diaphragm, it can cause pain in the shoulder tip, especially while lying down. This is a classic indicator of bleeding or discomfort inside the abdomen.
- Rapid Heart Rate (Tachycardia) and Low Blood Pressure: Fast heart rate (tachycardia) and low blood pressure are signs that you might be going into shock because of internal bleeding or a serious illness.
If you have a known hydrosalpinx and experience any of these hydrosalpinx rupture symptoms, seek emergency medical care immediately.
Is it Necessary to Remove Hydrosalpinx? Exploring Treatment Imperatives
This leads us to the most important question: “Is it necessary to remove hydrosalpinx?” Treatment is very personal and depends on things like the woman’s age, desire to get pregnant, severity of the condition, and whether it’s unilateral or bilateral hydrosalpinx. However, the overwhelming evidence points to surgery (specifically salpingectomy) as the best option, especially for women who want to get pregnant:
- Salpingectomy (Surgical Removal of the Tube): Salpingectomy, or surgical removal of the tube, is the most common and recommended treatment, especially before trying IVF.
- Why take it out? It gets rid of the source of the harmful fluid that hurts embryos and makes IVF less likely to work. After salpingectomy for hydrosalpinx, studies reveal a huge rise in the frequencies of IVF pregnancies and live births.
- Procedure: Most of the time, it is done laparoscopically, which is a minimally invasive way. Carefully pull the afflicted tube away from the rest of the body and take it out. It doesn’t take long to get better
- Bilateral Hydrosalpinx: If both tubes are broken beyond repair (bilateral hydrosalpinx), both tubes are usually taken out. This implies that natural conception is no longer possible, but it makes IVF far more likely to work by getting rid of the hazardous fluid reflux
- Reducing the Risk of Cancer: Recent studies also suggest that removing damaged fallopian tubes (a technique called opportunistic salpingectomy) may lower the risk of getting ovarian cancer later in life, as certain malignancies are now thought to start in the tube.
- Tubal Occlusion (Blocking the Tube Near the Uterus): Blocking the tube near the uterus, or tubal occlusion, is an option for some people who are having IVF instead of having it removed. Laparoscopy blocks the tube near the uterus, for example, with clips or cauterization. This stops the harmful fluid from flowing back into the uterus, which makes IVF more likely to work without having to remove the tube. It is not done as often as salpingectomy, although it may be an option in some cases.
- Aspiration (emptying the Fluid): Just emptying the fluid from the hydrosalpinx (with ultrasound guidance or during surgery) is not a good or long-term therapy. The fluid almost always comes back soon, and it doesn’t fix the damage to the tubes or the hazardous environment. It doesn’t help with fertility outcomes.
- Antibiotics: Only used to control the acute phase of an active illness (pyosalpinx or TOA). Antibiotics alone won’t fix the harm or obstruction that a chronic hydrosalpinx causes.
Living with Hydrosalpinx
Getting a diagnosis of hydrosalpinx can be hard on the emotions, especially for women who want to get pregnant. It’s very important to:
- Get Professional Help: Talk to a gynecologist who specializes in infertility or surgery on the reproductive system. They can give you the most accurate diagnosis, talk to you about all of your treatment options (such as salpingectomy vs. tubal occlusion), and help you choose the best way to reach your goals.
- Know Your Options: Be informed on what unilateral vs. bilateral hydrosalpinx means, how it affects natural fertility, how treatment is needed for IVF to work, and what the procedures are (such as laparoscopic salpingectomy).
- Take care of your emotional health: infertility and long-term illnesses can be hard on you. Get help from your spouse, family, friends, a therapist, or a support group.
- Focus on Fertility Solutions: If you want to get pregnant, know that hydrosalpinx makes it very hard to get pregnant naturally, but IVF is a very successful way to do it with the right treatment (typically removing the tubes). After the intervention, the success rates go up a lot.
- Make your overall pelvic health a priority: work with your doctor to treat any underlying problems, such as endometriosis or chronic pelvic pain.
Conclusion: Knowledge is Power, Don’t Ignore Hydrosalpinx
Hydrosalpinx is more than simply a plugged tube; it’s a serious disorder that can have a big impact on fertility and pelvic health. The first step to feeling empowered is to learn what hydrosalpinx is, what causes it (like PID and endometriosis), and what it could mean for you, especially the effects of bilateral hydrosalpinx and the answer to the important question, “How serious is hydrosalpinx?” Knowing that there is a chance of serious problems, such as the urgent hydrosalpinx rupture symptoms, shows why being careful is so important.
The evidence is clear about “Is it necessary to remove hydrosalpinx?”: For women who want to get pregnant, especially through IVF, surgery (usually salpingectomy) is not only helpful, but often critical to increase the chances of success and protect health.
Not paying attention to hydrosalpinx can ruin your chances of getting pregnant and cause problems that could have been avoided. If you have chronic pelvic pain, infertility, or have been told you have this problem, you should consult a doctor right away.
Taking charge of your health, making smart choices, and getting the right treatment can help you reach your family-building objectives and improve your health. Don’t let a blocked tube get in the way of your future. Take control of your reproductive health now.



[…] like severe pelvic inflammatory disease (PID) that damage the tubes, addressing blockages or hydrosalpinx (a fluid-filled tube), and removing benign growths or cysts. However, recent discoveries in gynecologic oncology have […]