About 1 in 10 people who were born female have endometriosis, which is a complicated and often devastating disorder. But its effects are still not well understood, even by doctors. The stages of endometriosis are one aspect that usually confuses people. Getting a diagnosis is a big step, but hearing that you have “Stage I” or “Stage IV” endometriosis frequently makes you want to know more. What do these phases of endometriosis mean? Does a higher stage mean more pain?
And most importantly, what does each Stage feel like in real life when you have this disease? This page provides in-depth details on the American Society for Reproductive Medicine (ASRM) staging system. It goes beyond clinical descriptions to look at how people with endometriosis live with it, the many symptoms they have, and how each Stage can have a significant effect on their physical, mental, and social health. It’s essential to understand the various stages of endometriosis, not only to facilitate a diagnosis but also to comprehend what patients are experiencing and assist them in selecting the most suitable treatment.
Why Stage Endometriosis? Understanding the ASRM System
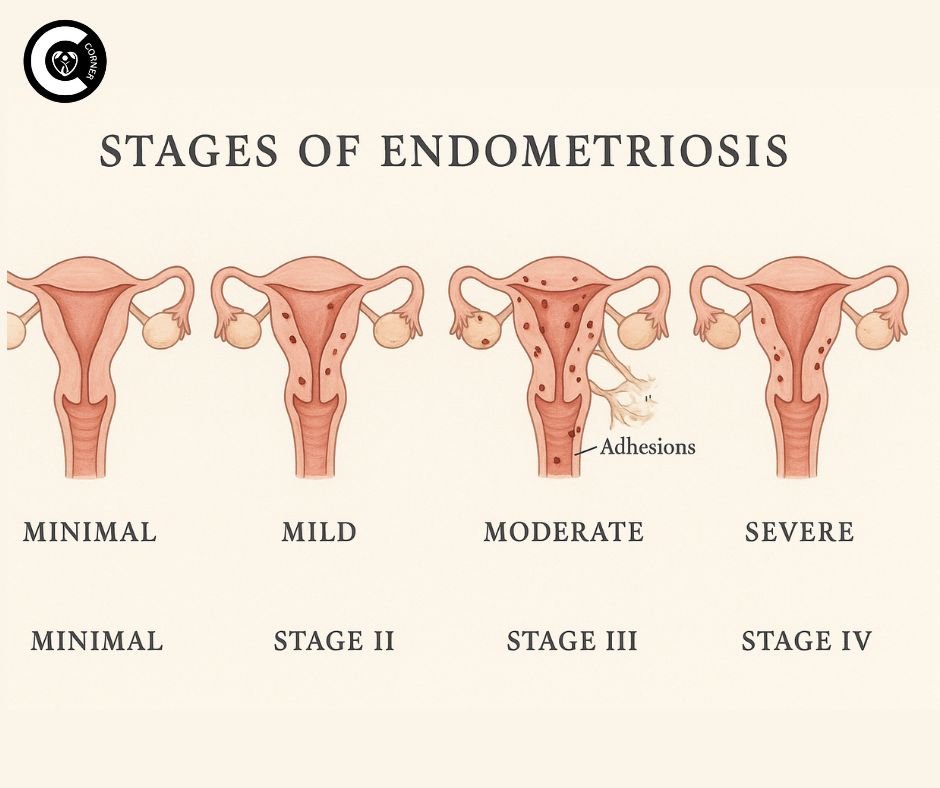
It’s essential to understand why staging occurs and its limitations before delving into the details of the various stages of endometriosis. The ASRM classification is the most common method for categorizing endometriosis into four stages: Minimal (Stage I), Mild (Stage II), Moderate (Stage III), and Severe (Stage IV). During laparoscopic surgery, the surgeon carefully notes down this staging:
- Location: Where does the endometriosis show up? (ovaries, peritoneum, uterine sacral ligaments, bowel, bladder, diaphragm, etc.)
- Extent/Amount: How many separate lesions or implants are there?
- Depth: How far into the surfaces or organs has the tissue spread? (Superficial vs. deep infiltrating endometriosis—DIE).
- Presence and Type of Endometriomas: Are there ovarian cysts with old blood in them (commonly dubbed “chocolate cysts”)?
- Adhesions: Are there bands of scar tissue holding organs together? How bad and thick are they?
Based on these variables, points are assigned, and the total score indicates the Stage of endometriosis the person is in. It’s essential to remember that the Stage is primarily determined by the extent and location of the disease in the body at the time of surgery, rather than the severity of a person’s pain or symptoms. This is one of the most significant gaps in understanding the stages of endometriosis. A person with Stage I disease may have agonizing, life-changing pain, while a person with Stage IV may have few symptoms at first, which are commonly found by accident during infertility tests. This complexity underscores the importance of listening to the patient’s experience, regardless of the Stage of surgery they’re in.
Breaking Down the Four Stages of Endometriosis: A Clinical Overview
What are the different stages of endometriosis? The ASRM system identifies four official stages of endometriosis. Let’s quickly go over the clinical features of each one:
- Stage I (Minimal): This Stage is marked by a few superficial implants (lesions on the surface of tissues), mainly on the pelvic lining (peritoneum) or surrounding pelvic organs. There is very little or no scar tissue (adhesions). At this point, endometriomas are relatively uncommon.
- Stage II (Mild): There are more implants than in Stage I, but they are still primarily on the surface and may go deeper. You might find these implants on the ovaries and the lining of the pelvis. Some minor adhesions may begin to form.
- Stage III (Moderate): There are numerous deep implants on the lining of the pelvis and ovaries. There are often one or more tiny endometriomas (usually less than 4 cm) on one or both ovaries. Dense adhesions are easily visible and may connect organs, such as the ovaries, to the pelvic wall or each other.
- Stage IV (Severe): This indicates that the disease has spread widely. It is normal to have many deep implants and big endometriomas (frequently more than 4 cm) on one or both ovaries. Numerous thick, strong adhesions often tie together the pelvic organs, including the ovaries, fallopian tubes, colon, bladder, and uterus. Implants can also be found in areas such as the appendix, the surface of the colon, or even farther away, like the diaphragm.
Now that we’ve reviewed the surgical notes, let’s discuss what it’s really like to live with each Stage of endometriosis.
Stage I Endometriosis (Minimal): Small Lesions, Potentially Big Pain
What it Looks Like Surgically
A few small patches or specks of endometrial-like tissue that are not deep, mainly on the pelvic peritoneum. Consider small areas instead of large ones. There are very few, if any, adhesions. Most of the time, the ovaries look normal.
How It Often Feels
Don’t be fooled by the word “minimal.” Stage I endometriosis can be very painful. The discomfort often doesn’t match up with how bad the disease looks. Why? Inflammation is significant. Even small implants can release chemicals that cause inflammation, which can lead to nerve pain and increase sensitivity in the pelvic area. Pain comes and goes, with a lot of it happening shortly before and during your period (dysmenorrhea). It could feel like:
- Intense, Sharp Cramping: These aren’t simply “bad period cramps.” They are excruciating, knife-like aches down in the belly or pelvis that commonly spread to the lower back or thighs.
- Ovulation Pain (Mittelschmerz) on Steroids: The pain can be terrible and last for days.
- Stabbing Pains with Bowel Movements or Urination: Sharp pains when going to the bathroom or having a bowel movement, especially around the time of your period, as the implants are located near the colon or bladder.
- Deep Ache or Heaviness: A continuous, nagging pain in the pelvis.
- The “Am I Crazy?” Phase: This is one of the most challenging stages to diagnose before surgery. Healthcare providers, friends, and family sometimes brush off symptoms as “just bad periods” or stress. People who are in pain may feel invalidated and upset, and they may even doubt their ability to feel pain. It’s usual to feel tired and have mood swings because of the inflammatory process and changes in hormones.
Fertility Considerations
Things to think about when trying to get pregnant: Stage I endometriosis is believed to be less likely to create structural problems, but it can still compromise fertility by causing inflammation that affects the quality of eggs, the function of sperm, or the implantation of embryos. At this point, unexplained infertility is not unusual.
Fertility Considerations
“My doctor kept saying my ultrasounds were clear, so it must just be IBS or anxiety. But the pain during my period was so bad that I would curl up on the bathroom floor and throw up. Getting diagnosed with Stage I felt good, but also confusing. How could something so ‘minimal’ cause so much pain? It turns out those tiny spots were setting my whole pelvis on fire.”
Stage II Endometriosis (Mild): Expanding Footprint, Intensifying Symptoms
What it Looks Like Surgically
There are more implants than in Stage I. Some of them may still be superficial, but others may begin to penetrate deeper into the tissues below the peritoneum. Lesions often show up on the ligaments that hold the uterus in place (such as the uterine sacral ligaments), the ovaries, and the pelvic sidewalls. Filmy adhesions may begin to form, causing the pelvic tissues to move slightly or adhere to each other.
What it Often Feels Like: The Grip Tightens
Stage II endometriosis symptoms often get worse, more frequent, and less predictable than those of Stage I. The deeper implants and early adhesions start to make the structure more sensitive and irritated:
- Increased Severity and Duration of Period Pain: Cramps may start days sooner and stay longer, so you may need greater pain medication or have to limit your activities a lot.
- Chronic Pelvic Pain (CPP): The pain may not only happen during your period. A dull discomfort or pressure that persists in the lower abdomen, back, or pelvis becomes a constant presence.
- Painful Sex (Dyspareunia): Deep penetration can cause acute, searing, or throbbing discomfort. This can happen because of implants on the uterosacral ligaments, the back of the vagina (cul-de-sac), or because of early adhesions that draw on the ovaries. This has a significant effect on relationships and closeness.
- Bowel and Bladder Symptoms Amplify: Around the time of your period, you may experience more urgency, frequency, pain when your bladder or bowel is full, bloating, and changes in your bowel habits (diarrhea or constipation). The soup that causes inflammation affects adjacent organs.
- Increased Fatigue and Brain Fog: The body’s ongoing fight against inflammation requires a significant amount of energy, making it harder to think clearly.
Fertility Considerations
The likelihood of having trouble getting pregnant goes up. Adhesions can gradually alter the function or movement of the tubes or ovaries. Inflammation is still a big deal.
Patient Perspective
“The pain started to affect my daily life. I dreaded sex because it hurt so much afterward. It was always bloated and had to go to the bathroom, especially around my period. I had no energy. Hearing ‘mild’ after surgery felt like a slap; this didn’t feel mild at all. The doctor explained the deeper implants and adhesions, and all of a sudden, it made more sense.”
Stage III Endometriosis (Moderate): Cysts, Scarring, and Significant Impact
What it Looks Like Surgically
At this Stage of endometriosis, the illness is more advanced. There are numerous deep implants. One of the most significant signs is that endometriomas, often referred to as “chocolate cysts,” are frequently found on one or both ovaries. These cysts are typically less than 4 cm in diameter but are nonetheless significant. Dense adhesions become more pronounced, further altering the shape of the pelvis. The ovaries could be attached to the pelvic wall or the rear of the uterus. The tubes could be kinked or only partially blocked. The rectum or bladder may also show signs of involvement.
What it Often Feels Like: The Weight of Adhesions and Cysts
Stage III endometriosis sometimes makes symptoms worse because of the actual presence of cysts and the straining, tugging, and tightness caused by extensive adhesions:
- Persistent and Severe Pelvic Pain: The pain is generally persistent, with significant flare-ups around ovulation and menstruation. The deep, gnawing pain is everywhere.
- Distinct Ovarian Pain: Endometriomas can cause a deep, throbbing, or intense pain that is just on one or both sides of the pelvis, especially while moving, having sex, or going to the bathroom. They can also make you feel heavy or as if you need to use the bathroom.
- Severe Dyspareunia: Deep penetration is typically quite uncomfortable. When adhesions tug on organs, they provide a painful, tearing feeling.
- Pronounced Bowel and Bladder Issues: Painful bowel movements (dyschezia), severe bloating (“endo belly”), constipation, diarrhea, rectal bleeding during menstruation, bladder pain, urgency, and frequency become more common and disruptive. Adhesions or rectal implants may cause bowel movements to feel blocked or incomplete.
- Sciatic Pain or Leg Pain: If implants or adhesions press on nerves near the sacrum or sciatic nerve, they can cause pain to radiate down the legs.
- Profound Fatigue and Systemic Symptoms: The fatigue is so bad that it takes control. A lot of people feel sick, have headaches, and feel nauseous. The inflammatory load is high.
Fertility Considerations
The chances of getting pregnant are much higher. Endometriomas can hurt the tissue in the ovaries and lower the number of eggs available. Adhesions can block or change the shape of the fallopian tubes, make it harder for the egg to be picked up, or stop ovulation. Inflammation is still having a harmful effect.
Patient Perspective
“Finding out I had endometriomas explained the constant deep ache in my side. The bloating was insane, I looked pregnant some days. Going to the bathroom during my period was a nightmare; it felt like passing glass. And the fatigue… it was bone-deep. ‘Moderate’ sounded right; this was a whole new level of disruption. The adhesions were pulling everything out of place.”
Stage IV Endometriosis (Severe): Widespread Disease and Complex Challenges
What it Looks Like Surgically
This is the most advanced Stage of endometriosis. It has numerous thick adhesions that often make it challenging to visualize normal pelvic anatomy. This is called a frozen pelvis because it binds organs together. Having more than one big endometrioma (>4 cm) is common. Many deep penetrating implants go deep into structures including the bladder wall, ureters, bowel wall, rectovaginal septum (the tissue between the vagina and the rectum), and maybe even beyond the pelvis (for example, the diaphragm or appendix). There is clear evidence of significant scarring and deformation.
What it Often Feels Like: The Unrelenting Storm
People with Stage IV endometriosis frequently have very bad, long-lasting, and complicated symptoms that affect many parts of their bodies. Pain is often continuous and makes it hard to do things:
- Constant, Severe Pelvic and Abdominal Pain: There is a deep, grinding, or crushing ache that is always there and is much worse when you move, sit, or put any weight on your abdomen.
- Bowel Obstruction-Like Symptoms: Deep bowel implants and dense adhesions can produce severe constipation, painful straining, ribbon-like feces, a feeling of not being able to empty the bowels fully, and sometimes nausea or vomiting, especially around the time of menstruation. There is a chance of bleeding from the rectum.
- Urinary Tract Issues: Bladder implants can cause severe bladder pain (like interstitial cystitis), a strong need to urinate, frequent urination, pain when the bladder is full, and sometimes blood in the urine (hematuria) regularly. Involvement of the ureters (which is rare but significant) can cause the kidneys to enlarge (hydronephrosis).
- Excruciatingly Painful Sex: Deep penetration is often impossible because of pain from adhesions, fixed organs, and deep implants. A light touch can hurt.
- Cyclical Shoulder or Chest Pain: If you have diaphragmatic endometriosis, you may feel pain in your shoulder or upper abdomen, especially around your period. This discomfort may be accompanied by shortness of breath or pain when you take a deep breath.
- Severe Fatigue and Debilitation: The persistent pain, swelling, and possible nutritional deficiencies (resulting from bowel problems) leave people feeling exhausted, making it difficult to perform everyday duties and their job.
Fertility Considerations
Natural conception is typically very hard because of a lot of adhesions, damage to the tubes and ovaries from large or recurring cysts, and the overall messed-up pelvic environment. IVF and other assisted reproductive technologies (ART) are often needed.
Patient Perspective
“It felt like my insides were glued together in a painful knot. Sitting was painful. A simple bowel movement could make me cry and leave me tired. My bladder felt like it was on fire all the time. The pain went beyond my pelvis; every month, I’d get stabbing pains in my shoulder. ‘Severe’ was an understatement. It took over my whole life. Surgery was complicated and took a long time to heal, but it was necessary to get some function back.”
The Crucial Disconnect: Why Stage Doesn’t Equal Pain
It is essential to reiterate: the Stage of endometriosis found during surgery does not accurately predict the intensity of discomfort or specific symptoms a person experiences. Patients and doctors alike find this to be one of the most frustrating aspects of the disease.
- Stage I Sufferers: They can feel pain that is just as bad as someone with Stage IV. The amount of nerve density in the affected areas, central sensitization (when the nervous system becomes hypersensitive), the exact location of the implants (for example, on very sensitive nerves), and each person’s pain threshold are all crucial factors.
- Stage IV Patients: If the disease is in places with fewer nerves or hasn’t generated a lot of inflammation or nerve irritation that sends out constant pain signals, they may have remarkably bearable pain. They might be diagnosed because they can’t have kids, or by chance during another procedure.
- The Takeaway: The main point is that your pain is real, regardless of the Stage of surgery you’re in. A “minimal” stage finding does NOT suggest that your pain is minor or made up. On the other hand, being in a “severe” stage doesn’t always indicate your pain will be too much to handle (though it does often suggest your symptoms are more complicated). Not just the stage number, but also your symptoms and goals (such as pain relief, preserving fertility, etc.) should be the primary focus of treatment.
Conclusion: Validation, Understanding, and Empowerment
Understanding the various stages of endometriosis provides a foundation, but it’s not the entire story. Pain, exhaustion, and interruption are more than just numbers on a scale. How many levels of endometriosis are there? Four. What are the different stages of endometriosis? Very little, a little, a lot, or a lot. However, what each Stage feels like is a profoundly personal experience of living with a sickness that is often hard to foresee, invisible, and misunderstood.
If you think you have endometriosis or if your existing diagnosis doesn’t match how much pain you’re in, speak up for yourself. Look for doctors who listen to you, understand the complexities of endometriosis, and are dedicated to treating you, not just a number on a surgical report. They should be concerned about your symptoms, your objectives, and your overall quality of life. The best opportunity for a significant improvement is through laparoscopy and professional excision. Keep in mind that your pain is real, what you’re going through is real, and you can get better. Understanding the stages of endometriosis empowers you to ask the right questions and receive the care you need.

[…] of ovulation pain, what is completely normal, what may indicate an underlying condition such as endometriosis ovulation pain, and how it links to fertility, is critical for peace of mind and proactive health […]