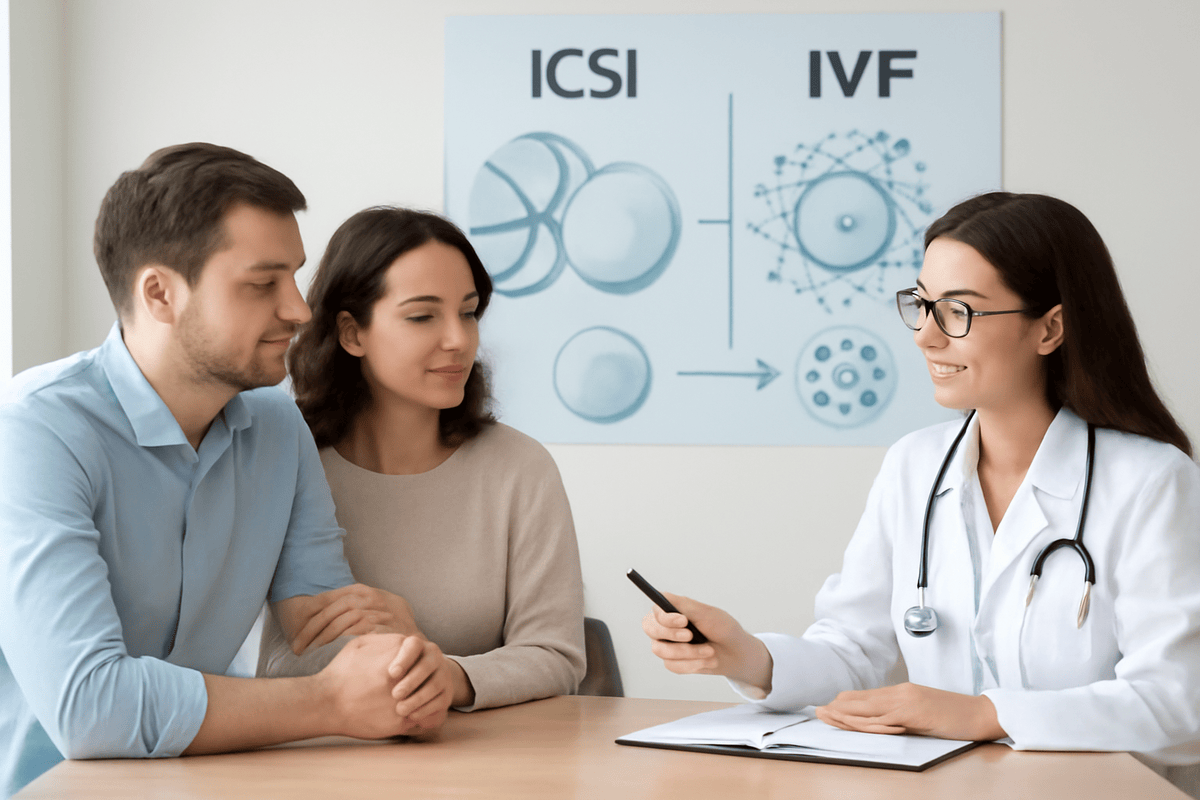
Embarking on the path to parenthood is one of life’s most profound journeys. For many, this road leads to the world of Assisted Reproductive Technology (ART), a landscape filled with hope, advanced science, and a sometimes-confusing array of acronyms. Two of the most common and successful treatments are ICSI and IVF. If you’re wondering about the difference between ICSI vs Conventional IVF, you’re not alone. This comprehensive guide is designed to demystify these procedures, compare ICSI vs IVF success rates, and empower you with the knowledge to have informed conversations with your fertility specialist about which path might be right for you.
Understanding the Basics: What is IVF?
Before we dive into the ICSI vs IVF comparison, it’s crucial to understand the foundation upon which both are built: In Vitro Fertilization (IVF).
The IVF Process Step-by-Step
In Vitro Fertilization, which literally means “fertilization in glass,” is a multi-step process that has helped millions of families worldwide. Conventional IVF involves bringing the magic of conception into the embryology lab.
1. Ovarian Stimulation: The patient undergoes hormone injections to stimulate the ovaries to produce multiple mature eggs, rather than the single egg typically released in a natural cycle.
2. Egg Retrieval: Once the eggs are mature, a minor surgical procedure is performed to collect the eggs from the ovarian follicles.
3. Sperm Collection: On the same day as the egg retrieval, a sperm sample is provided by the male partner or a donor.
4. Fertilization in the Lab: This is the critical step where Conventional IVF and ICSI differ. In Conventional IVF, the embryologist places thousands of motile sperm in a petri dish with each egg. The sperm compete naturally to penetrate and fertilize the egg on its own.
5. Embryo Development: The fertilized eggs (now embryos) are monitored for growth and development over 3-5 days.
6. Embryo Transfer: One or more healthy embryos are selected and transferred into the woman’s uterus through a thin catheter.
7. The Two-Week Wait & Pregnancy Test: After the transfer, you wait approximately two weeks before taking a blood test to confirm pregnancy.
Diving Deeper: What is ICSI?
Now, let’s explore the more precise technology that is often used alongside IVF: Intracytoplasmic Sperm Injection (ICSI).
The ICSI Procedure: A Precision Micro-Injection
ICSI (pronounced “ick-see”) is not a replacement for IVF; it is a specialized form of it. Think of ICSI vs IVF not as a choice between two separate journeys, but as a choice between two different fertilization techniques within the IVF process. The initial steps, ovarian stimulation, egg retrieval, and embryo transfer, are identical. The difference lies solely in how the egg is fertilized. In the ICSI procedure, an embryologist uses high-powered microscopes and incredibly delicate micromanipulation tools. They carefully select a single, morphologically normal sperm and immobilize it. Then, using an ultra-fine glass needle, they directly inject that single sperm right into the cytoplasm (the center) of the egg. This bypasses the need for the sperm to swim to the egg, penetrate its outer layers, and trigger fertilization naturally.
ICSI vs Conventional IVF: A Head-to-Head Comparison
The core difference in the ICSI vs Conventional IVF debate is the method of fertilization. But this fundamental difference leads to several key distinctions.
| Feature | Conventional IVF | ICSI |
|---|---|---|
| Fertilization Method | Natural selection: Sperm and eggs are placed together, allowing fertilization to occur naturally. | Manual selection: A single sperm is directly injected into each mature egg. |
| Sperm Requirement | Requires a good number of motile, morphologically normal sperm. | Can be performed with very few sperm, even with severe male factor infertility. |
| Primary Use Case | Female factor infertility, unexplained infertility, fallopian tube issues. | Male factor infertility, previous IVF fertilization failure, using frozen sperm. |
| Level of Intervention | Less invasive at the fertilization stage. | Highly invasive micromanipulation of the egg and sperm. |
When is Conventional IVF Typically Recommended?
Conventional IVF is often the first-line approach when:
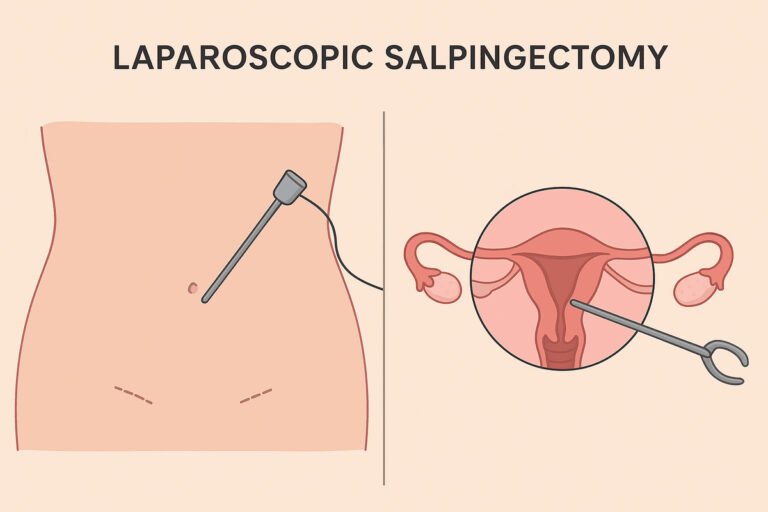
- The primary fertility challenges are on the female side (e.g., blocked fallopian tubes, endometriosis, ovulation disorders).
- There is unexplained infertility.
- The male partner’s semen analysis is within normal ranges for count, motility (movement), and morphology (shape).
When is ICSI Typically Recommended?
ICSI was developed to overcome male factor infertility and is strongly recommended in these scenarios:
- Severe Male Infertility: Very low sperm count (oligospermia), poor sperm motility (asthenospermia), or abnormal sperm morphology (teratospermia).
- Previous IVF Failure: If a prior cycle of Conventional IVF resulted in failed or very low fertilization.
- Surgical Sperm Retrieval: When sperm is obtained directly from the testicles (e.g., via TESA or TESE) due to an obstruction or absence of the vas deferens. These samples often contain very few, immotile sperm.
- Preimplantation Genetic Testing (PGT): ICSI is often used alongside PGT to ensure no extra sperm are attached to the egg’s outer shell, which could contaminate the genetic sample taken from the embryo.
- Using Frozen Eggs or Donor Sperm: ICSI can sometimes be opted for to maximize fertilization success with these materials.
Analyzing ICSI vs IVF Success Rates
This is often the most pressing question for intended parents. So, which has higher ICSI vs IVF success rates? The answer is more nuanced than a simple “this one is better.”
Fertilization Rates: The Initial Hurdle
For couples with male factor infertility, ICSI success rates for fertilization are significantly higher than Conventional IVF. By manually injecting the sperm, ICSI overcomes the sperm’s inability to penetrate the egg. In cases of severe male factor, Conventional IVF may result in little to no fertilization, while ICSI can achieve fertilization rates of 70-80%.
For couples without male factor issues, studies show that ICSI and IVF success rates for fertilization are generally comparable. Some studies even suggest that Conventional IVF might have a slight edge, as it allows for the natural selection of the most potent sperm.
Clinical Pregnancy and Live Birth Rates
When it comes to the most critical outcome, taking a healthy baby home, the data is reassuring. For couples with male factor infertility, ICSI unequivocally leads to higher pregnancy and live birth rates because it enables fertilization to occur.
For couples without a diagnosed male factor, extensive research has shown that ICSI does not necessarily result in higher pregnancy or live birth rates compared to Conventional IVF. If the sperm parameters are normal, both methods are equally effective in achieving a successful pregnancy. Therefore, performing ICSI “just in case” without a medical indication may not offer any added benefit.
Boosts Testosterone Levels Naturally with Ashwagandha
Weighing the Pros and Cons: ICSI and IVF
Both procedures come with their own sets of advantages and considerations.
Advantages of ICSI
- Overcomes Severe Male Infertility: This is its primary and most powerful benefit.
- High Fertilization Rate: Minimizes the risk of total fertilization failure.
- Enables Use of Retrieved Sperm: Makes parenthood possible for men with obstructive azoospermia.
Considerations for ICSI
- Cost: ICSI adds cost to the overall IVF cycle due to the highly skilled labor and specialized equipment required.
- Theoretical Risks: Because ICSI bypasses natural selection, there were initial concerns about passing on genetic issues related to male infertility or causing damage to the egg. However, decades of use have shown ICSI to be very safe. The absolute increased risk of congenital disabilities is minimal and is often linked to the underlying infertility itself rather than the ICSI procedure. Genetic counseling is recommended for severe male factor cases.
Advantages of Conventional IVF
- Less Invasive: Does not involve physically penetrating the egg.
- Lower Cost: Less expensive than an IVF cycle that includes ICSI.
- Natural Selection: Allows for the “Survival of the fittest” sperm to fertilize the egg.
Considerations for Conventional IVF
- Risk of Fertilization Failure: There is a chance, even with normal sperm, that fertilization may not occur, which can be emotionally and financially devastating.
- Not an Option for Male Factor: Will not work for couples with significant male infertility diagnoses.
Making the Decision: Which One is Right for You?
The choice between ICSI and IVF is not one you make alone. It is a deeply personal medical decision that should be made in close consultation with your fertility doctor based on a comprehensive diagnostic workup of both partners.
Key Factors Your Doctor Will Consider
- Semen Analysis Results: This is the most critical factor. Your doctor will meticulously review the count, motility, and morphology of the sperm.
- Your Fertility History: Have you had previous IVF cycles? If so, what was the fertilization rate?
- Female Partner’s Age and Ovarian Reserve: While related to overall IVF success, this can influence how aggressively your doctor wants to pursue the best fertilization method.
- Plan for Genetic Testing: If you are doing PGT, your clinic will likely recommend ICSI.
Ask your doctor
- “Based on our semen analysis, do we medically require ICSI?”
- “What have been your clinic’s ICSI vs IVF success rates for patients with a similar profile to ours?”
- “What are the added costs and benefits of ICSI in our specific situation?”
Conclusion: Your Personalized Path to Parenthood
The journey to conceive is unique for every individual and couple. Understanding the difference between ICSI and IVF is a decisive step in taking control of your fertility treatment. Remember, ICSI vs Conventional IVF is not about one being universally better than the other. It is about which tool is right for your specific diagnosis.
Conventional IVF remains a fantastic, less invasive option for many, particularly those facing female factor or unexplained infertility. ICSI, on the other hand, is a revolutionary technique that has opened the doors to parenthood for countless couples facing male factor infertility.
Inflammation and Infection: Leading Causes of Painful Ejaculation
Ultimately, trust in the expertise of your medical team, advocate for yourself by asking questions, and know that by understanding these processes, you are already navigating your parenthood journey with strength, knowledge, and hope. Your path is your own, and with today’s advanced technology, including both ICSI and IVF, that path has more possibilities than ever before.