Imagine an incessant, distressing physical sensation in your most intimate regions, arousal that you did not request, do not desire, and are unable to manage. It endures for hours, days, or even indefinitely, resulting in profound shame, exhaustion, and isolation, rather than the delight it was intended to bring. This is the harsh reality for those who are living with Persistent Genital Arousal Disorder (PGAD). This condition is profoundly misunderstood and frequently concealed, shrouded in silence. PGAD is a distinct form of suffering that many individuals endure alone, in disbelief, as it is intrusive, unwanted, and disconnected from desire, in contrast to typical sexual arousal.
This article breaks the silence by providing a comprehensive and empathetic examination of PGAD disorder. Also, it includes symptoms, the challenging path to diagnosis, potential treatment avenues for PGAD, and strategies for reclaiming life amidst this invisible battle. You are not alone if you have ever had the question, “Do I have PGAD?”. We explore the science, the lived experience, and the hope that exists beyond the stigma.
What Exactly Is PGAD Disorder?
Persistent Genital Arousal Disorder (PGAD) is a complex neurophysiological condition. Also called Persistent Sexual Arousal Syndrome (PSAS) or Restless Genital Syndrome (ReGS), it primarily affects individuals assigned female at birth. A persistent, intrusive sensation of genital arousal that is not associated with feelings of sexual desire defines the characteristic of PGAD disorder.
These sensations are extremely distressing, involuntary, and spontaneous. The arousal sensations in PGAD are not relieved by orgasm and may worsen temporarily afterward. This creates a cruel paradox for those affected. This absence of resolution is a critical distinction from conventional sexual arousal. The sensations are persistent and cause severe psychological distress. This includes anxiety, depression, shame, and a loss of bodily control. To comprehend PGAD, it is necessary to transcend simplistic concepts of “being on.”
PGAD is a neurological malfunction, an intrusive physiological state that disrupts a person’s well-being and sense of self. It severely impacts daily life, relationships, and mental health. PGAD is profoundly isolating. Many sufferers stay silent, fearing their symptoms will be misunderstood or dismissed.
Recognizing PGAD Symptoms
PGAD symptoms are often difficult to recognize and describe. Yet, identifying them is crucial for getting help. The manifestations are not limited to mere physical sensations; they comprise an intricate web of anguish:
The Core Physical Experience
“PGAD’s defining feature is persistent, unwanted sensations in the genital area, such as the clitoris, labia, vagina, perineum, or anus. Less commonly, it may also affect the nipples. These sensations are commonly described as feelings of engorgement, fullness, pressure, vibration, pulsation, humming, or tingling. These sensations are unwelcome, unprovoked by sexual thoughts or stimuli, and cause substantial distress.
The Orgasm Paradox
Contrary to conventional arousal, the sensations are not alleviated by the attainment of an orgasm, whether through masturbation or partnered intercourse. Often, orgasm brings only brief relief or, worse, intensifies arousal afterward. This traps sufferers in a cycle of despair. This absence of resolution is a defining and particularly cruel characteristic of PGAD.
Triggers and Amplifiers
Although the sensations occur spontaneously, specific activities or states can frequently exacerbate or initiate PGAD symptoms. Stress and anxiety, which can perpetuate a vicious cycle, prolonged sitting (such as during work commutes or desk jobs), vibrations (from vehicles or machinery), friction from clothing, urinary fullness, sexual stimulation (even if unwanted at the time), and specific phases of the menstrual cycle are all common triggers. It is crucial to identify personal triggers to manage PGAD disorder effectively.
The Psychological and Emotional Toll
The unrelenting physical sensations undoubtedly result in severe psychological repercussions. Social isolation is prevalent due to the fear of symptoms manifesting in public, the inability to participate in typical activities, and the apprehension of having to explain the inexplicable. Sufferers frequently experience intense anxiety, panic attacks, profound depression, overwhelming shame, guilt, and feelings of being “broken” or “dirty.” Sleep deprivation is a prevalent issue, as sensations frequently become more intense during the night or while at rest. Comprehensive care for PGAD is essential due to the significant cumulative influence on quality of life, relationships, work, and overall mental health.
Potential Causes and Risk Factors: Unraveling the Mystery of PGAD Disorder
The precise causes of PGAD are still under investigation, and they are multifactorial, meaning that a combination of factors can contribute to or converge in an individual. It is essential to comprehend potential contributors to facilitate the assessment and treatment of PGAD:
Neurological Factors
The evidence is compelling and suggests that the causes are neurological or dysregulated. Potential mechanisms consist of:
- Nerve Entrapment/Injury: Pudendal neuralgia, a nerve that serves the genital region, is frequently associated with PGAD. This condition is characterized by irritation or compression of the pudendal nerve. Nerves can be damaged by injuries resulting from surgery (particularly pelvic surgeries such as hysterectomy), childbirth, cycling, or trauma.
- Spinal Cord Issues: Nerves involved in genital sensation can be irritated by Tarlov cysts (fluid-filled sacs on nerve roots at the base of the spine), cauda equina involvement, or other spinal abnormalities.
- Central Sensitization: The nervous system may become hypersensitive, causing an increase in the intensity of normal sensations to a distressing level. This phenomenon is potentially associated with conditions such as fibromyalgia or chronic pelvic pain.
- Dopaminergic Dysregulation: It is suspected that imbalances in brain chemicals, such as dopamine, which are involved in reward and motor control pathways, may be to blame.
Vascular Factors
The sensations of engorgement and pressure encountered in PGAD have been proposed to be influenced by abnormalities in blood flow to the genital region.
Medication Side Effects or Withdrawal
The emergence or exacerbation of PGAD symptoms has been associated with the use of specific medications, particularly certain antidepressants (SSRIs/SNRIs), when they are initiated, adjusted, or discontinued. Hormonal treatments may also contribute to the issue.
Hormonal Influences
In certain individuals, fluctuations in hormones, particularly during specific menstrual cycle phases, perimenopause, or menopause, can induce or exacerbate PGAD. Nerve function and tissue integrity are believed to be impacted by low estrogen levels.
Psychological Factors
Although PGAD is not predominantly a psychological disorder, the substantial distress it induces has a considerable effect on mental health. Pre-existing conditions, such as anxiety, OCD, or a history of sexual trauma, may potentially lower the threshold for developing PGAD or exacerbate the experience; however, they are not the primary cause. The relentless physical symptoms of PGAD disorder are the cause of the psychological toll, not the other way around.
Do I Have PGAD? Navigating the Complex Path to Diagnosis
The inquiry “Do I have PGAD?” is both legitimate and reasonable if you are experiencing persistent, distressing genital sensations that correspond to the descriptions above. Accurate diagnosis of PGAD disorder is notoriously tricky and frequently necessitates a protracted, discouraging process:
1. Locating the Appropriate Healthcare Provider
This is frequently the most significant obstacle. PGAD is not well-known or understood by a substantial number of gynecologists, urologists, or general practitioners. Consult with providers who specialize in urogynecology, neurology, pelvic discomfort (such as pelvic floor physical therapists), or sexual medicine. Online or through patient advocacy organizations, such as the International Society for the Study of Women’s Sexual Health (ISSWSH), research specialists are readily accessible.
2. The Critical Medical History
Be prepared for sensitive, exhaustive inquiries. A comprehensive history, which encompasses the following, is required by your provider:
- A detailed account of your sensations, including their location, quality, intensity, and duration.
- The date on which it began and any potential precipitating events (e.g., surgery, injury, medication change).
- The factors that contribute to its improvement or detriment (triggers, relieving factors).
- The effect of an orgasm (relief, deterioration, or no change).
- Your hormonal status and menstrual cycle.
- Complete medication and supplement history.
- History of pelvic surgeries, trauma, or childbirth.
- Additional medical conditions (e.g., neurological issues, spinal problems, pelvic pain, mental health).
- The profound emotional and life-altering effects.
3. Comprehensive Physical Examination
A sensitive pelvic assessment is typically necessary to exclude other conditions during a comprehensive physical examination. This may evaluate the tone of the pelvic floor muscles (hypertonicity is a common symptom of PGAD), detect indications of nerve pain (such as allodynia, which is pain that occurs with light contact), and examine for infections, skin conditions, or anatomical abnormalities. Additionally, it is crucial to conduct a neurological examination that evaluates sensation and reflexes in the legs and pelvis.
4. Diagnostic Tests (Ruling Out Mimics)
There is no singular test for PGAD. The primary method of diagnosis is clinical, relying on the exclusion of other conditions and the assessment of symptoms to determine the underlying cause. Examinations may encompass the following:
- Urinalysis and cultures to exclude urinary tract infections.
- Pelvic ultrasound to detect vascular issues, fibroids, or lesions.
- MRI of the pelvis, lumbar, and sacral spine to detect nerve compression (e.g., pudendal neuralgia, Tarlov cysts), spinal concerns, or other abnormalities.
- Blood tests to determine hormone levels, thyroid function, and rule out systemic ailments.
- Nerve conduction investigations (less common, occasionally employed when pudendal neuralgia is suspected).
5. The Importance of Validated Criteria
Providers must consult established diagnostic criteria, such as those proposed by the International Society for the Study of Women’s Sexual Health (ISSWSH). A critical prerequisite is that the sensations induce significant interpersonal conflict or distress. Persistence is also essential; symptoms must be present for a substantial period (e.g., at least three months).
6. Patience and Persistence
The process of diagnosing a condition may require months or even years. Even if one provider dismisses you, do not give up. Obtain second, third, or fourth opinions from specialists who are well-informed and meticulously document your symptoms. It is of the utmost importance to locate a provider who is willing to investigate PGAD, believes in you, and actively listens to you. The self-advocacy and fortitude necessary to answer the question “Do I have PGAD?” are immense.
Current PGAD Treatment Approaches and Strategies
Although there is no universal cure for PGAD disorder, effective PGAD treatment focuses on managing symptoms, reducing distress, and enhancing quality of life. The treatment is highly individualized and often requires a multi-modal approach specifically designed to address the suspected underlying cause(s). Patience and perseverance are essential:
Addressing the Root Causes (If Identifiable)
- Pudendal Neuralgia: Treatments may include targeted pelvic floor physical therapy (PT), pudendal nerve blocks (injections of anesthetic and corticosteroid), pulsed radiofrequency ablation, or surgical decompression in severe, refractory cases.
- Tarlov Cysts: Management encompasses surgical drainage or repair for symptomatic cysts, as well as monitoring for asymptomatic cysts.
- Medication Triggers: It is essential to collaborate with a psychiatrist to modify or replace a suspected medication, such as an SSRI. Antidepressants should never be discontinued abruptly.
- Hormonal Factors: Hormone replacement therapy (HRT), particularly vaginal estrogen, may alleviate symptoms in peri/menopausal individuals by enhancing nerve function and tissue health. Balancing additional hormones may also be investigated.
Pharmacological Interventions (Symptom Management)
Neuropathic Pain Medications
Drugs such as pregabalin (Lyrica) or gabapentin are frequently prescribed as the initial treatment to alleviate overactive nerves. Tricyclic antidepressants (e.g., nortriptyline, amitriptyline) may also be beneficial for neuropathic pain and may improve sleep.
- Oral muscle relaxants (e.g., baclofen, cyclobenzaprine) or compounded vaginal medications containing muscle relaxants may be beneficial in the presence of pelvic floor hypertonicity.
- SSRIs/SNRIs: Although they are occasionally associated with the development of PGAD, certain types or concentrations (e.g., a higher dose of escitalopram) may paradoxically alleviate symptoms by modulating neurotransmitters. However, this necessitates meticulous expert supervision.
- Antipsychotics (Low Dose): Medications such as aripiprazole (Abilify) or quetiapine (Seroquel) in extremely low concentrations may reduce intrusive sensations and modulate dopamine pathways, particularly in the presence of OCD-like features.
- Benzodiazepines (Short-term): Clonazepam or diazepam may be used judiciously to treat severe anxiety or panic attacks, but their long-term use is generally discouraged due to dependency risks.
Nonpharmacological therapies
- Pelvic Floor Physical Therapy (PT): Required for the majority. A specialized physical therapist evaluates the tension, strength, and coordination of the pelvic floor muscles. The treatment consists of manual therapy (both internal and external), myofascial release, trigger point release, biofeedback, stretching, relaxation techniques, and home exercises to restore muscle function and alleviate nerve irritation. PT is frequently a fundamental component of treating PGAD.
- Transcutaneous Electrical Nerve Stimulation (TENS): The application of low-voltage electrical currents through pads located near the afflicted area can occasionally disrupt pain/arousal signals.
- Cognitive Behavioral Therapy (CBT) and mindfulness: The psychological impact is significantly mitigated through therapy. CBT assists in the development of coping skills for distress and anxiety, the challenge of negative thought patterns, and the resolution of any associated sexual concerns or trauma history. The immediate intensity of sensations can be managed through the use of mindfulness and grounding techniques.
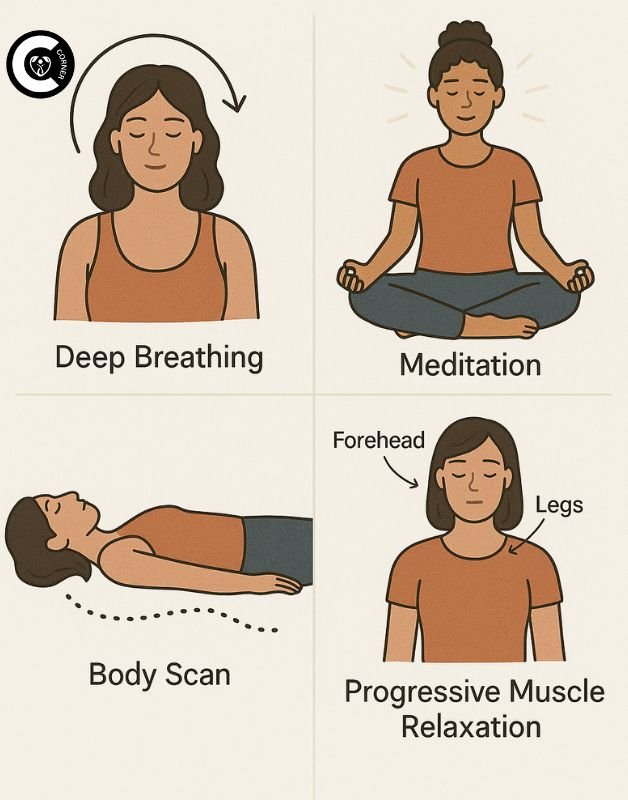
- Lifestyle Modifications: It is essential to identify and avoid personal triggers, such as certain sitting positions, tight clothing, caffeine, and tension. Occasionally, applying ice compresses to the skin can temporarily numb sensations. Managing stress through yoga, meditation, or gentle exercise, as well as maintaining proper sleep hygiene, are also critical supportive strategies for managing symptoms of PGAD.
Finding Hope and Moving Forward With PGAD
Living with PGAD disorder is an arduous journey that is characterized by physical pain, emotional distress, and frustrating conflicts within the healthcare system. Requiring significant self-advocacy and resilience, the journey to identifying an effective treatment for PGAD can be lengthy and convoluted. However, optimism endures in the face of this challenging situation. The landscape is gradually evolving: a robust, supportive online community provides connections and validation, a growing number of healthcare providers are educating themselves, and research is progressing steadily.
Although a universal cure may not be imminent, numerous individuals can achieve effective symptom management and substantial improvements in their quality of life by adopting a persistent, multidisciplinary approach tailored to their circumstances. If you identify with these descriptions of PGAD symptoms, please be aware that your suffering is genuine, valid, and warrants compassionate care. You are not alone, and you are not damaged. Continue to seek out knowledgeable providers, investigate the variety of treatment options, prioritize your mental health, establish connections with individuals who share your perspective, and tenaciously guard your optimism.
The initial step toward a future in which this “silent struggle” is no longer mute is to break the silence surrounding PGAD. This silence will be replaced with understanding, effective treatments, and unwavering support. Asking the question “Do I have PGAD?” and seeking answers are essential steps toward obtaining the care you deserve. By doing so, you may experience relief and a renewed sense of control.




[…] Also read: Mindfulness and relaxation techniques for managing PGAD symptoms and reducing stress […]