Many women must deal with dyspareunia, which is pain during sex. This is a very prevalent but generally unspoken problem for many women after menopause. If intimacy has become linked with discomfort, scorching, aching, or even tearing feelings, remember that this is not an unavoidable aspect of ageing, nor something you must silently bear. Painful sex has a big effect on relationships, self-esteem, and the quality of life as a whole. There are important solutions that work. This article goes into great detail on what doctors want women to know about painful sex after menopause. It talks about the causes, the different medical and lifestyle treatments that are available, and the powerful message that it is possible to have comfortable, pleasant intimacy again. The first step to getting your sexual health back is to figure out why you’re in discomfort.
Understanding Dyspareunia
Dyspareunia refers to persistent or repeated genital pain that occurs immediately before, during, or after sexual intercourse. It happens a lot more often during the transition to menopause and beyond menopause. It is a complicated ailment that usually comes with big changes in the body and sometimes changes in the mind as well. The pain can be anything from a burning or stinging feeling at the vaginal opening (entrance dyspareunia) to a deep aching or pressure feeling in the pelvis (deep dyspareunia) to a general soreness. If you ignore uncomfortable sex, it won’t go away; in fact, it may get worse over time, which can lead to a cycle of avoidance, worry, muscle tension (vaginismus), and even more pain. It is very important to see it as a real medical illness that has to be treated.
Why Menopause Triggers Painful Intercourse
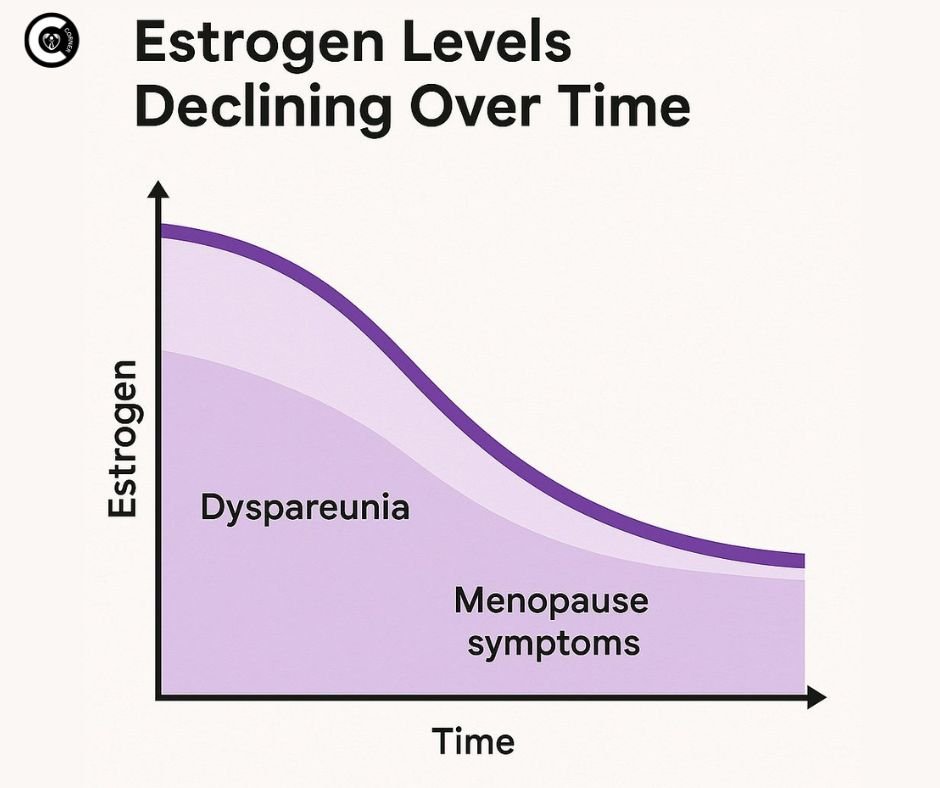
The main reason why sex hurts after menopause is that estrogen levels drop so much. Estrogen is very important for keeping the vagina and vulva healthy. It keeps the vaginal tissues thick, stretchy, well-lubricated, and full of blood. During perimenopause, estrogen levels drop sharply, and they stay low after menopause. This causes big alterations in the tissues, which are now named genitourinary syndrome of menopause (GSM) instead of vulvovaginal atrophy (VVA). GSM includes the thinning (atrophy), dryness, and swelling of the vaginal walls, vulva, and urethra. This makes tissues that are weak, less elastic, easily irritated, and don’t make as much natural lubricant. Even light friction during sex can produce micro-tears, inflammation, burning, and a lot of pain, which is a sign of postmenopausal dyspareunia. The main cause is loss of estrogen, although other things often make it worse.
Also Read : Role Of Niacin In Erectile Dysfunction
Recognizing the Symptoms
Dyspareunia presents in diverse forms beyond the acute discomfort of intercourse. Knowing about these related symptoms can aid with diagnosis and show that GSM is a systemic problem:
- Persistent Vaginal Dryness: feeling dry all the time, not just during sex.
- Burning or Itching: Burning or itching, especially around the vulva and the opening of the vagina.
- Stinging Sensation: Especially when urinating (dysuria) or when urine touches inflamed tissues.
- Light bleeding or spotting: This might happen after sex since the tissues are weak and tear.
- Urinary Symptoms: More frequent, urgent, or recurrent urinary tract infections (UTIs) because the urethra is getting thinner and the pH is changing.
- Tightness or Narrowing: The feeling that the vaginal aperture has gotten narrower or tighter.
- Less arousal and libido: Pain naturally lowers sexual desire and the body’s natural arousal reaction.
- General Discomfort: Experiencing soreness, rawness, or irritation in the vulvovaginal region, even in the absence of sexual activity. It is important to recognize this group of symptoms in order to get the right therapy for painful sex after menopause.
Reclaiming Comfort: Effective Treatments for Dyspareunia
The good news is that there are many successful treatments for painful sex after menopause, both hormonal and non-hormonal. The best way to treat your condition is frequently with a combination therapy that is based on your individual reasons, health profile, and preferences.
Hormonal Therapies: Addressing the Root Cause (Low Estrogen)
- Vaginal Estrogen Therapy (First-Line Treatment): This is the best way to treat dyspareunia that is related to GSM. Creams (like Premarin or Estrace), tablets or inserts (like Vagifem or Imvexxy), or a soft ring (Estring) that is worn all the time give low-dose estrogen directly to the vaginal tissues. It reduces systemic absorption (very little gets into the bloodstream) while successfully repairing the thickness, flexibility, blood flow, and lubrication of vaginal tissue, maintaining a healthy pH, and lowering the risk of infection. Most of the time, painful sex gets better in a few weeks to a few months. Most women can safely use it, even those who have had hormone-sensitive malignancies in the past (talk to your oncologist).
- Vaginal DHEA (Prasterone): Intrarosa is an insert that contains dehydroepiandrosterone (DHEA), a hormone that is converted in modest amounts into estrogen and testosterone by vaginal cells. It works well to alleviate painful sex after menopause with few side effects on the body as a whole.
- Ospemifene (Oral SERM): Ospemifene (Osphena) is a Selective Estrogen Receptor Modulator (SERM) that you take once a day. It functions like estrogen on vaginal tissues, making them thicker and more slippery, but it stops estrogen from working in the breast. It’s another good way to treat dyspareunia throughout the body.
- Systemic Hormone Therapy (HT/MHT): If you are also having serious menopausal symptoms, including hot flashes, night sweats, or worries about losing bone mass, systemic HT (estrogen +/- progesterone, depending on whether you have a uterus) might be an option. It helps with symptoms all over the body, but it especially helps with vaginal health and uncomfortable sex. Talk to your doctor in depth about the risks and advantages.
Non-Hormonal Treatments: Important Tools for Relief
- Regular vaginal moisturizers: These long-lasting remedies (including Replens, Hyalo Gyn, and Good Clean Love Restore) keep vaginal tissues hydrated and help keep the pH level healthy. This reduces baseline dryness and irritation that can lead to dyspareunia.
- Lubricants (Crucial for Sex!): To reduce friction and pain during sex, you must use a lot of water-based (like Astroglide or Liquid) or silicone-based (like Uberlube or Pjur) lubricants. Stay away from things that can irritate your skin, like glycerin, parabens, flavors, or warming/cooling ingredients. Oil-based lubes, such as coconut oil and pure silicone, work well but can damage latex condoms.
- Pelvic Floor Physical Therapy (PFPT): A key treatment, especially if muscular tension (vaginismus) or weakness is a problem. A physical therapist who specializes in pelvic floor muscles offers exercises (such as focused Kegels, relaxation techniques, and stretching), employs manual treatment, and may use biofeedback or dilators to retrain the muscles, minimize spasms, enhance function, and make sex less painful after menopause. Using smooth, medical-grade dilators of increasing size over time is part of dilator therapy. This helps desensitize tissues and gently extend the vaginal canal.
- Treating Infections & Skin Conditions: It’s important to treat any underlying BV, yeast infections, or skin problems (such as lichen sclerosis, which is treated with strong topical steroids) very carefully.
- MonaLisa Touch & Other Laser/Energy Therapies: These fractional CO2 or Erbium YAG lasers are meant to get vaginal tissues to make more collagen and blood flow. Some women say that these treatments help with GSM symptoms and painful sex, but they are expensive, typically need several sessions, and insurance doesn’t always cover them. Also, we don’t yet know how safe and effective they are in the long term compared to conventional therapy like vaginal estrogen. Talk to your doctor about it in detail.
- Cognitive Behavioral Therapy (CBT) and Sex Therapy: Helps with the worry, fear, negative thoughts, and relationship problems that come with dyspareunia. Therapists give people ways to deal with how they feel pain, talk to their partners better, make sex more intimate without penetration, and have more positive sexual experiences.
Lifestyle & Self-Care: Empowering Yourself Daily
Proactive self-care, when combined with medical therapies, greatly increases comfort and lessens unpleasant sex after menopause:
- Prioritize Regular Sexual Activity/Self-Stimulation: Getting sexually aroused on a regular basis, with or without a partner, improves blood flow to the pelvic tissues, which helps keep them healthy and lubricated. “Use it or lose it” is a good way to remember that mild, pleasurable stimulation keeps tissue supple. Using a dilator also fits into this group.
- Avoid Irritants: Don’t use strong soaps, douches, scented hygiene products, bubble baths or tight synthetic pants. For the vulva only, use a mild, fragrance-free cleanser like Cetaphil. The vagina cleans itself. After swimming in pools with chlorine, make sure to rinse off well.
- Stay Hydrated: Drinking enough water keeps your body hydrated, especially your mucous membranes.
- Choose Cotton Underwear: It lets air flow better, which cuts down on moisture buildup and irritation.
- Communicate Openly with Your Partner: Talk to Your Partner Honestly: Talk about your pain in an open, honest, and non-blaming way. Try non-penetrative ways to be intimate that are fun and don’t hurt, such as massage, reciprocal masturbation, oral sex, and sensual touch. Work together to find the right pace, lubricant, and postures that make you feel less pain.
- Manage Stress: Long-term stress can make pelvic tension worse. Add relaxing methods like deep breathing, yoga, or meditation.
- Avoid Smoke: Smoking makes blood flow worse, which makes vaginal tissue health worse and dyspareunia worse.
Conclusion: Hope, Help, and Healthy Relationships Wait
Dyspareunia after menopause is a prevalent, manageable medical condition, not a life sentence or an unavoidable result of ageing. Knowing how important estrogen decrease (GSM) and other variables are helps explain why sex hurts after menopause. There are many very effective therapies available, such as localized vaginal estrogen and moisturizers, pelvic floor therapy, and open communication tactics. Relief is possible. You may get back to having comfortable, meaningful intimacy and greatly improve your overall health by speaking out, getting a full diagnosis, and being an active part of your treatment plan. You should have a satisfying sex life no matter how old you are. Talk to your doctor immediately to take the first step. There is hope and treatment available.




[…] Also Read: Painful Intercourse After Menupause […]
[…] Also Read: How To Get Rid Of Painful Intercourse After Menopause […]
[…] Painful Sex (Dyspareunia): Deep penetration can cause acute, searing, or throbbing discomfort. This can happen because of implants on the uterosacral ligaments, the back of the vagina (cul-de-sac), or because of early adhesions that draw on the ovaries. This has a significant effect on relationships and closeness. […]
[…] ovulation pain is commonly described as more intense, lasts longer, and may be accompanied by deep pain during intercourse (dyspareunia), painful bowel motions (dyschezia), or chronic pelvic pain outside of ovulation. If you feel your […]
[…] and severe pain. This can show up as debilitating pelvic pain, painful periods (dysmenorrhea), painful sex (dyspareunia), infertility, chronic fatigue, and stomach problems like bloating, constipation, or […]