If you’ve recently had your intrauterine device removed and are experiencing unexpected bleeding, you might be wondering whether it’s a red flag or just part of the process. Could this be a sign of a problem, or is your body simply adjusting? Let’s explore the facts to help ease your concerns. Some bleeding is expected, but heavy bleeding may not always be normal. In most cases, light spotting or mild cramping happens after removal. But if you’re soaking through pads or experiencing dizziness or clots, it could signal something else, like hormonal withdrawal, infection, or uterine changes.
Understanding Your IUD: Copper vs. Hormonal
Before discussing the bleeding, it is essential to understand the two primary types of Intrauterine Devices (IUDs) and the fundamental differences between them within the uterus. This distinction is crucial for understanding the distinct effects of each on your menstrual bleeding.
The Copper IUD (Non-Hormonal)
A minute quantity of copper wire encircles this diminutive, T-shaped device. The primary mechanism of action is the release of copper ions into the uterine cavity. These ions create an environment that is detrimental to sperm, thereby hindering the fertilization process. Copper IUDs mustn’t contain any hormones. As a result, they typically do not suppress ovulation or significantly alter your natural hormonal cycle. Nevertheless, the inflammatory response induced by the copper and the presence of a foreign object can have a substantial impact on the lining of your uterus and the blood vessels.
The Hormonal IUD (Progestin-Releasing)
This IUD, which is also T-shaped, consistently releases a very low concentration of a synthetic progestin hormone (such as levonorgestrel) directly into the uterine lining. This hormone has multiple effects: it thickens cervical mucus, which prevents sperm from entering the uterus; thins the endometrium, thereby thinning the uterine lining; and can occasionally suppress ovulation, particularly when used in higher doses. Even though the hormonal IUD’s primary objective is to decrease menstrual flow over time, the initial adjustment period may involve irregular spotting or bleeding.
The insertion of an IUD is a brief but significant event. A clinician uses a specialized inserter to deliver the device through the cervix and ensure it is appropriately positioned within the uterine cavity. This physical act can result in immediate spotting or cramping by causing transient trauma to the cervical tissue and the endometrium.
Why Does IUD Insertion Cause Heavy Bleeding?
The initial period of spotting or bleeding that occurs immediately following the insertion of an IUD is nearly universally accepted as usual. However, what is the cause of this phenomenon, and when does it transition into problematic excessive bleeding?
- Physical Trauma: The uterine lining is touched by the instruments used during insertion, including the speculum, uterine sound, and inserter tube, which travel through the sensitive cervical canal. This will inevitably result in minor abrasions or irritation, which may cause light bleeding or discoloration for a few days. Consider it a minor injury within.
- Foreign Object Reaction: The uterus is a sterile environment. The introduction of any foreign object initiates a localized inflammatory response, whether it be a copper IUD or a hormonal IUD. This is the body’s innate defense mechanism activating. This inflammation can result in the fragilization and leakage of blood vessels, which can contribute to spotting or light bleeding, as white blood cells race to the area. This inflammatory response is more severe for specific individuals.
- Uterine Adjustment: The uterus is a contractile organ. Intense menstrual symptoms may result from the placement of a device within it, as the muscles contract in response to the presence of the new object. Additionally, these contractions may induce bleeding and aggravate the lining.
This initial hemorrhaging typically resolves within 3 to 7 days for most individuals. Nevertheless, persistent or unusually excessive bleeding following the insertion of an IUD, particularly beyond the initial week, is indicative of a potential underlying issue, frequently associated with the specific type of IUD you have.
The Copper IUD Conundrum: Why Heavy Periods Are Common
If you have chosen the copper IUD and are currently experiencing periods that are significantly heavier, longer, or more painful, you are experiencing a prevalent, albeit frustrating, adverse effect. The copper IUD is virtually synonymous with excessive bleeding for a significant number of users, as outlined below:
The Pro-Inflammatory Effect
Copper is not inert within the body; instead, it actively induces a robust inflammatory response in the uterine lining. The endometrium becomes more vascular as a result of this chronic, low-grade inflammation, leading to the development of larger and sometimes more numerous blood vessels. Additionally, it increases the thickness of the lining in certain regions.
Interference with Clotting
The inflammatory chemicals released (prostaglandins) can disrupt the natural mechanisms that facilitate blood clotting within the uterine vessels during your period. This implies that hemorrhaging may be more intense and prolonged due to the additional time required for vessels to seal effectively.
Increased Uterine Contractions
The inflammatory response and the physical presence of the IUD can also induce more frequent and harsher uterine contractions (cramps). This sensation of gushing or inundation, which is associated with heavy bleeding after copper IUD insertion, can be attributed to the more forceful expulsion of blood and tissue by these intense contractions.
No Hormonal Suppression
Unlike the hormonal IUD, the copper version does not suppress ovulation or alter the endometrium. Your natural cycle, which includes the development and removal of a dense lining, continues unabated. The normal shedding process is merely exacerbated by the inflammation, resulting in a significantly heavier discharge.
Research consistently indicates that copper IUD users experience an average of 20-50% more menstrual blood loss, particularly in the initial 6-12 months. Although this improvement is often noticeable after the first year, periods frequently remain heavier than they were before the IUD was inserted for the duration of the device’s use. For individuals like me, this increase is not only apparent but also detrimental.
Hormonal IUDs and Bleeding: A Different (But Still Complex) Pattern
Although the hormonal IUD is frequently promoted as a solution for excessive menstrual bleeding, its initial effects can be perplexing and occasionally alarming. Do not be alarmed if your initial experience involves an increase in hemorrhage, rather than a decrease:
The Adjustment Phase (First 3-6 Months)
The synthetic progestin (levonorgestrel) requires time to affect the endometrium fully. The lining may initially become unstable due to the effects of this hormone. This instability results in irregular bleeding and spotting. You may experience mild bleeding daily, unpredictable spotting between periods, or episodes of heavy bleeding. This is a phenomenon that is exceedingly prevalent and typically transient.
Endometrial Thinning Takes Time
The primary mechanism for reducing bleeding is the progressive thinning (atrophy) of the uterine lining. This procedure is not completed overnight. The lining becomes so thin that there is very little tissue to shed as the progestin exposure persists month after month, resulting in lighter periods or even amenorrhea (no periods) for many users.
Spotting vs. Heavy Bleeding
Hormonal IUDs are less likely to experience sustained heavy bleeding, such as the need to saturate a pad or tampon every 1-2 hours for multiple hours, after the initial adjustment period, than copper IUDs. Nevertheless, episodes of heavier flow may occur during the adjustment phase. A visit to the doctor is necessary to exclude other potential causes or placement issues in the event of persistent excessive bleeding that persists for more than six months.
The primary message for hormonal IUD users is as follows: Patience is indispensable. This irregular hemorrhage pattern during the initial months is typically a result of your body’s adaptation to the treatment. For the majority of individuals, the issue is resolved, resulting in periods that are significantly lighter or nonexistent. Nevertheless, an investigation is necessary if there is substantial heavy bleeding that does not conform to the anticipated spotted pattern or does not improve.
Heavy Bleeding After IUD Removal
You ultimately determined that the intense bleeding following the insertion of a copper IUD was excessive, or you may have reached the end of the lifespan of your hormonal IUD. Removal is typically fast and significantly less irritating than insertion. Nevertheless, you may experience a recurrence of hemorrhage, occasionally with considerable intensity. For what reason?
Hormonal Rebound (Especially After Hormonal IUD)
Assuming you had a hormonal IUD, the consistent flow of progestin was actively inhibiting the growth of your endometrium. That suppression is eliminated upon its removal. The uterine lining can begin to regenerate swiftly as a result of your body’s natural estrogen production. If ovulation occurs relatively rapidly, you may experience a withdrawal flow, which may be followed by a potentially heavier-than-average “first real period” as your body ejects the lining that has accumulated without the IUD’s thinning effect.
Uterine/Cervical Irritation
The physical act of removal entails grasping the IUD strings and dragging the device through the cervical canal. This can result in minor trauma or irritation to the cervix and endometrium, which may produce mild bleeding or spotting immediately following removal and may persist for a few days.
Return to Your Natural Cycle
The inflammatory effect of a copper IUD likely caused your periods to be heavier while it was in position. The inflammation diminishes after its removal. Nevertheless, your “natural” period pattern resumes. If you had heavy periods before the IUD, you may revert to that level. Your body may require 1-3 cycles to achieve complete regulation.
Underlying Conditions Revealed
Occasionally, the IUD concealed an underlying condition that caused thick periods, such as fibroids or adenomyosis. The symptoms were under control while the IUD was in position, particularly a hormonal one that suppressed bleeding. The excessive bleeding that was caused by the underlying condition returns after it has been removed. This was a component of my “scary truth.”
While it is common to experience some spotting or a slightly heavier first period after IUD removal, persistent or exceptionally heavy bleeding (such as soaking pads hourly and passing large clots frequently) is not typical and should be monitored.
Coping with Heavy Bleeding After IUD
Persistent heavy menstruation following the insertion of an IUD is both emotionally and physically taxing. Here are strategies to manage it while you collaborate with your physician to identify the cause and long-term solutions:
Hydration is Essential
Fluid loss is a direct result of substantial blood loss. To maintain hydration and prevent fatigue, it is recommended to consume a sufficient amount of water and consider using electrolyte beverages (such as Pedialyte or diluted sports drinks).
Iron Supplementation
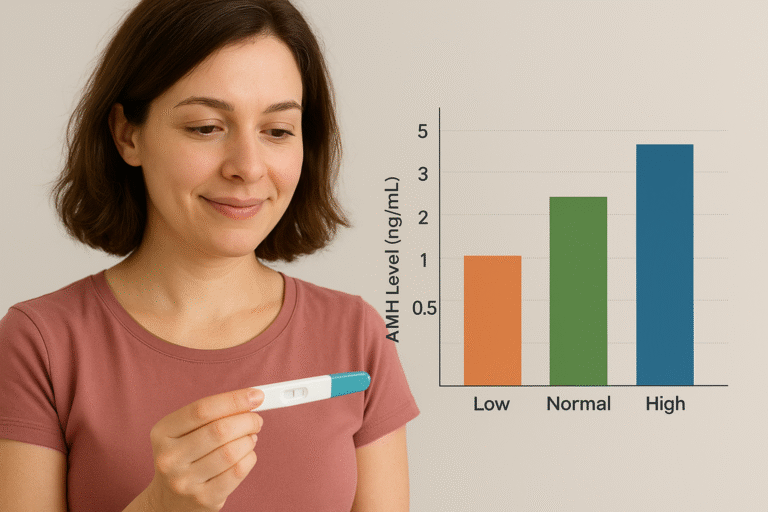
Iron deficiency anemia is primarily caused by heavy menstrual bleeding, which can lead to symptoms such as fatigue, lethargy, dizziness, and shortness of breath. Request that your physician conduct an iron level assessment (ferritin is the most reliable indicator). They may suggest an iron supplement. For improved absorption and fewer adverse effects compared to ferrous sulfate, consider a form such as ferrous bisglycinate.
Pain Management
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) such as Ibuprofen (Advil, Motrin) or Naproxen (Aleve) are your allies. In addition to alleviating cramping, they also decrease the production of prostaglandins, which can reduce menstrual blood flow by 20-50%. Administer them promptly upon the first indication of pain or bleeding, and continue to do so as prescribed.
High-Capacity Menstrual Products
Invest in options that are both reliable and highly absorbent.
- Menstrual Cups: Menstrual cups are capable of containing a substantially greater volume of fluid than tampons, with some models capable of holding up to 30 milliliters. Super Jennie, Merula XL, and Venus Cup are brands that are specifically engineered to accommodate high discharge rates.
- Period Underwear: Thinx, Knix, and Modibodi are among the brands that offer highly absorbent underwear, with some models capable of retaining up to 5-8 tampons’ worth of fluid. This type of underwear is suitable for secondary or occasional use on days that are not particularly demanding. Excellent for security during the night.
- Overnight Pads/Adult Diapers: For the most effective overnight protection and peace of mind, it is recommended to use the highest absorbency overnight pads or disposable incontinence underwear (such as Depends Silhouette or Always Discreet). Additionally, period-proof pajama bottoms may prove advantageous.
Monitor Your Bleeding
Use a period tracking application (such as Clue, Flo, or Spot On) to record the intensity of your flow (spotting, light, medium, heavy, or gushing), duration, pain levels, and any additional symptoms (such as fatigue or clots). This data is essential for discussions with your physician.
Rest and Listen to Your Body
Heavy bleeding can be tiring. Allow yourself additional time to relax. If you experience extreme fatigue or faintness, refrain from engaging in strenuous activities. Heating pads or warm baths may alleviate cramping.
Conclusion: Knowledge, Advocacy, and Hope
Heavy bleeding following the insertion of an IUD or even after its removal can be intimidating, isolating, and exhausting. Regardless of whether it is the anticipated inflammatory effect of a copper IUD, the adjustment phase of a hormonal IUD, or a warning sign of a more serious condition, such as adenomyosis (as in my case), it necessitates attention.
The Key Takeaway
Listen to your body. If your bleeding is so heavy that you’re soaking through pads or tampons every hour, passing large clots, or feeling dizzy and fatigued, it’s time to seek medical help. These could be signs of IUD malposition, infection, or an underlying condition like fibroids or adenomyosis (as in my case). Even if your doctor initially dismisses your concerns, advocate for yourself and ask for an ultrasound, blood tests, or further investigation.

[…] Heavy bleeding after IUD removal: normal? Ultimate Guide […]
[…] your attention. This small, flexible vaginal ring offers a unique balance between the pill and an IUD. However, before requesting a prescription from your healthcare provider, it is essential to be […]